My knee is locked!
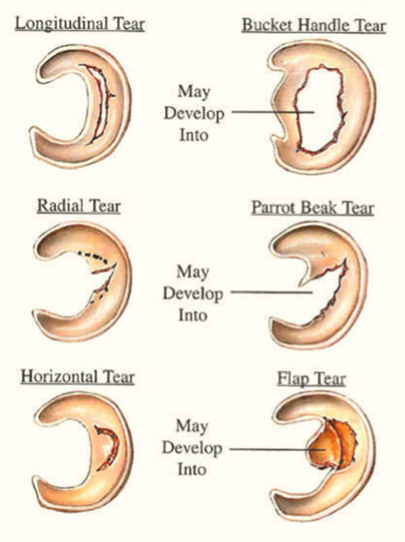
The knee joint is designed to bend up and down and rotate to a certain degree. If something gets caught inside the joint, it blocks the movement and the knee gets lock. The locked knee is most commonly as a result of a meniscus tear. Other causes of a locked knee are due to cartilage and bony fragments, ligament injury, loose tissue fragment and patella (knee cap) dislocation. In this article, I would like to focus on the meniscus injury as it is the most common cause of locked knee.
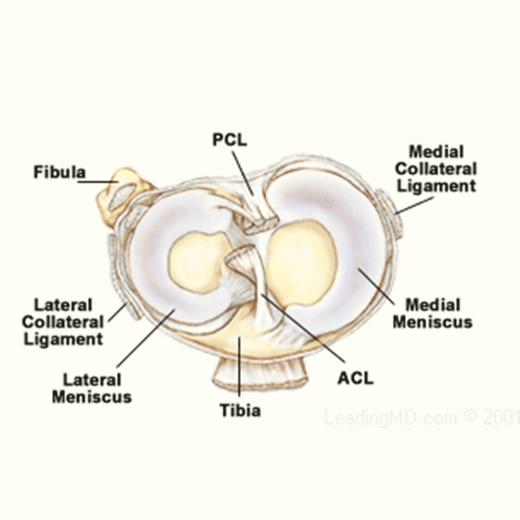
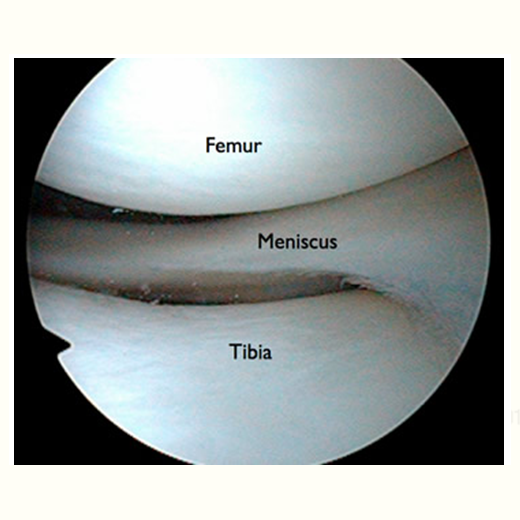
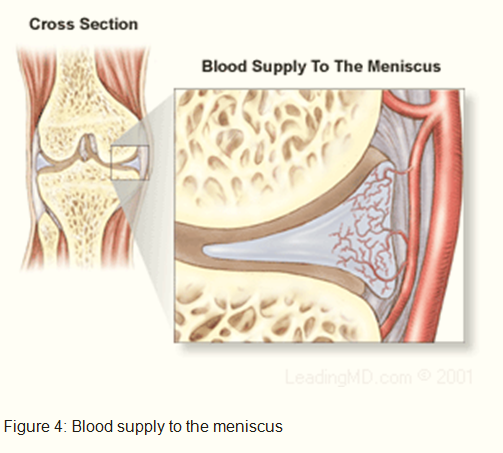
The meniscus is a rubbery, C-shaped cartilage in between the femur (thighbone) and tibia (shinbone). There are two menisci in each knee joint, the inner medial meniscus and the outer lateral meniscus. The outer edges are fairly thick while the inner surfaces are thin. The meniscus provides smooth knee motion, stability and contributes to a healthy knee through its shock absorber effect. During the various phases of the walking cycle, forces shift from one meniscus to the other, and forces on the knee can increase to 2 – 4 times body weight. While running, these forces on the knee increase up to 6 – 8 times body weight. There are even higher forces when landing from a jump.