Are mammograms really painful? Is 3D technology more effective at detecting breast cancer? SJMC Consultant Breast Surgeon Dr Teh Mei Sze clears up common misconceptions and shares preventive measures for breast cancer.

Dr Teh Mei Sze, Consultant Breast Surgeon (Oncoplastic) at Subang Jaya Medical Centre (SJMC), believes breast cancer screening has entered the era of personalised healthcare. Doctors must now consider a patient’s age, breast density, family history, and personal risk factors when recommending an individualised breast cancer screening plan.
Breast Cancer: A Growing Concern
According to 2020 data from the World Health Organization (WHO) , 2.3 million women globally were diagnosed with breast cancer, leading to nearly 670,000 deaths. In Malaysia, breast cancer remains a significant health threat, particularly among Chinese women.
Dr Teh Mei Sze stresses the importance of regular breast screenings: "In line with Malaysia’s breast cancer screening guidelines, individuals with a family history of breast cancer should begin mammograms at age 40, while those without a family history are advised to start at age 50. Follow-up exams should take place every 1-2 years, depending on personal circumstances. For women under 40, breast ultrasound is a suitable option."
She encourages everyone to make a habit of performing monthly self-examinations: “The purpose of self-examinations is to become familiar with your breasts, increase your awareness of breast health, and recognise what is normal for you. If you notice any changes in appearance or sensation, it’s crucial to consult a doctor promptly for further evaluation." Dr Teh highlights that self-examination complements professional examinations and imaging techniques but is not a substitute for them.
For any concerns about breast health or when facing a cancer diagnosis that requires treatment planning, it's advisable to consult with a breast or oncology specialist before making any significant decisions. Managing breast cancer often requires a multidisciplinary approach, involving surgeons, clinical oncologists, pathologists, and radiologists.

The Era of Personalised Healthcare in Breast Cancer Screening
With advances in cancer treatment and technology, a cancer diagnosis is no longer viewed as a death sentence. The rise of precision medicine has revolutionised cancer treatment, shifting away from a one-size-fits-all approach towards a focus on each patient’s unique genetic makeup, medical history, test results, and other characteristics. This personalised approach offers hope for more effective treatment and the potential for living with cancer.
In the past, all individuals, regardless of risk, followed the same screening protocol. Dr Teh believes breast cancer screening is now in a “personalised healthcare” era. While recommended screening ages in guidelines serve as a reference, the required tests can vary from person to person. Doctors should therefore consider factors such as age, breast density, and family history to recommend a tailored screening plan. This may involve flexible use of ultrasound, 3D mammography, and genetic testing (such as BRCA testing) to detect breast cancer early and ensure timely intervention.
Both breast screening and breast cancer treatment rely on early prevention, prompt diagnosis, and thorough planning to help individuals fight cancer effectively.
Debunking Myths about Breast Examinations
Myth #1: Mammograms are very painful, especially for women with smaller breasts.
Fact: Dr Teh clarifies that discomfort during a mammogram is not related to breast size or texture. While some pain may be experienced, it is usually brief and manageable. Breasts consist of glandular tissue and fat, and the proportion varies between individuals, as does pain tolerance.
Myth #2: I can just have a painless breast ultrasound instead of a mammogram.
Fact: There are three main breast screening methods: ultrasound, mammography, and MRI. Women should choose the appropriate method based on their age, family history of breast cancer, and pregnancy status. Dr Teh notes that women aged 20-40 typically have denser breast tissue, making ultrasound the primary screening method. However, it may not detect the calcifications that mammography can.
Myth #3: Breast cancer is hereditary, and I don’t need regular screenings as I have no family history.
Fact: This is a common misconception. While genetics play a role in some cases, only around 20% of breast cancer cases involve a family history. Environmental factors, lifestyle choices, obesity, and long-term smoking or drinking habits also contribute to breast cancer risk. Therefore, it is essential to perform self-examinations and undergo regular breast screenings to prevent and manage breast cancer.
Myth #4: Men don’t get breast cancer, so they don’t need breast checks.
Fact: Both men and women can develop breast cancer, although it is rare in men. Male breast cancer accounts for less than 1% of all cases. Early detection is vital for both men and women. If men notice any abnormalities, they should promptly consult a specialist for necessary examinations to detect breast cancer early and prevent it.
Myth #5: If I feel a lump in my breast, it means I have breast cancer.
Fact: It is common for women to have breast lumps, and most are benign, such as those caused by fibrocystic changes or fibroadenoma. Dr Teh advises against assuming cancer if a lump is detected. Instead, consult a doctor to determine the cause and appropriate next steps. She also addresses the misconception that a biopsy can cause cancer to spread: "A biopsy is the only way to diagnose whether a breast lump is cancerous, and the procedure is relatively simple. Doctors take a small sample of tissue for laboratory testing. A biopsy does not contribute to the spread of cancer."
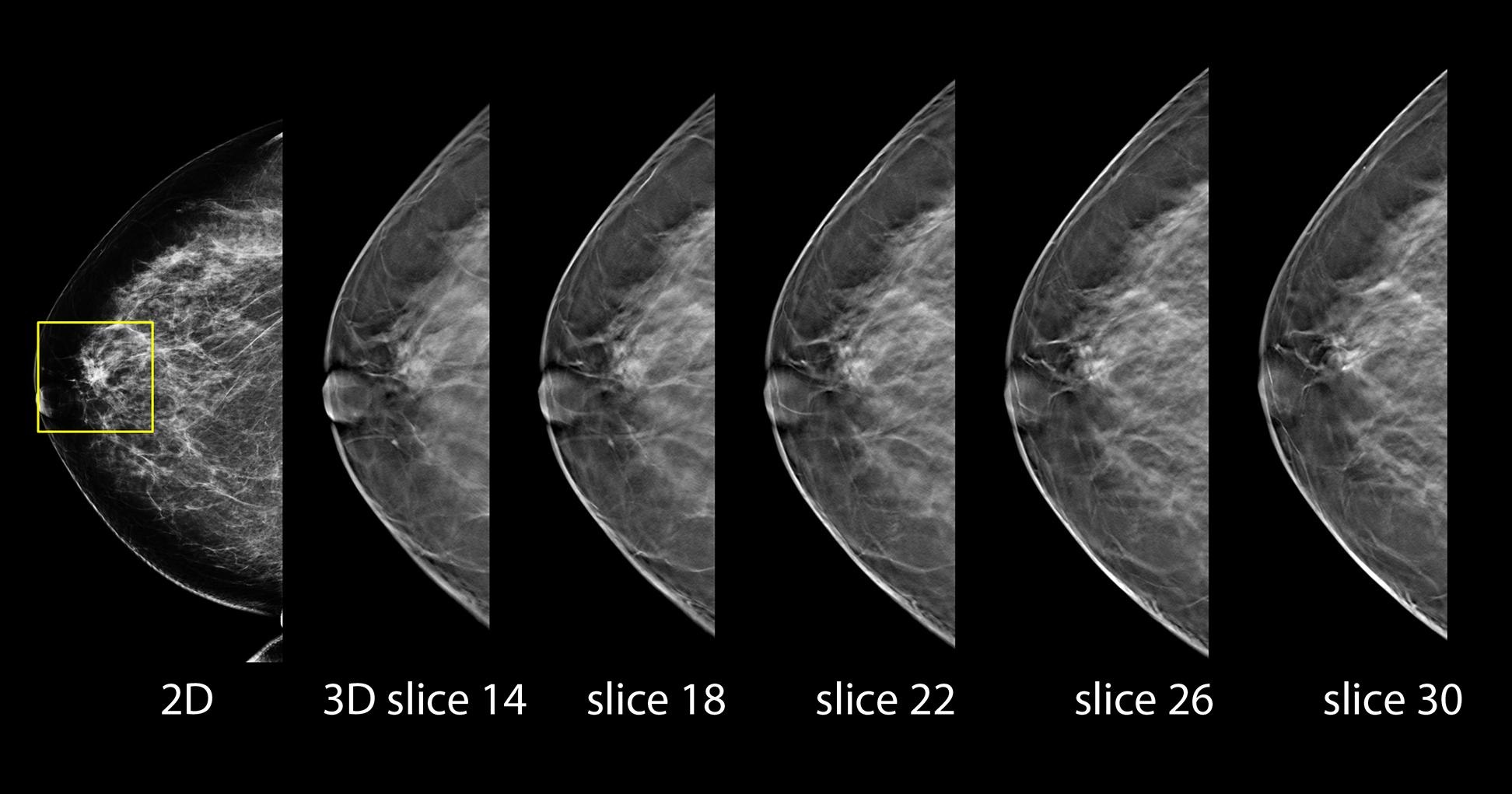
Comparison of 2D and 3D Mammography.
New Insights into Breast Screening: 3D Mammography
Breast cancer is challenging to prevent due to its complex causes, so the emphasis should be on early detection and treatment. Currently, mammography is the most effective breast cancer screening tool recommended by international research, as it can detect small, hidden lesions. Traditionally, mammography used 2D technology, but continuous advancements have significantly improved breast imaging.
3D mammography has recently emerged as a new trend in breast cancer screening. This imaging technology offers more detailed images, helping doctors make more accurate diagnoses.
To illustrate, 2D mammography is like looking at a book with all the pages stacked together, while 3D mammography allows doctors to examine breast tissue page by page. By capturing images from multiple angles and reconstructing them into a 3D dynamic image, doctors can better inspect each layer of breast tissue and locate hidden lesions. Although 3D mammography still requires compression to reduce breast thickness and enhance diagnostic accuracy, the technology can shorten the duration of compression and minimise discomfort.
Source: China Press