Prostate Cancer in Malaysia: What You Need to Know
Featuring Dr Peter Ng, Consultant Urologist, Subang Jaya Medical Centre (SJMC)
Prostate cancer is a significant health issue, ranking as the third most common cancer among Malaysian men. Traditional treatment methods often come with challenges, including long-term side effects that can impact a patient’s quality of life.
Men’s Health Awareness Month in June offers an ideal opportunity to educate and empower individuals about the latest advancements in prostate cancer treatment, encouraging proactive action for early detection.
In the recent CodeBlue Q&A with Dr Peter Ng, a consultant urologist from Subang Jaya Medical Centre (SJMC), we explore innovative advancements in prostate cancer treatment and the role of cutting-edge technology in revolutionising patient care.
New treatment methods focus on more precise targeting of tumours to minimise collateral damage, according to Dr. Ng. This means that advanced techniques are being developed to aim directly at the cancerous cells, reducing the risk of harming surrounding healthy tissues. These innovations are intended to make treatments safer and more effective, improving the overall quality of life for patients.

Newer treatment methods for prostate cancer aim to achieve more precise targeting of the tumour to reduce collateral damage, shared Dr Peter Ng.
Overview of Prostate Cancer in Malaysia
A study by Jasmine Ng and colleagues, based on data from nine public urology referral centres across Malaysia, revealed that between 2016 and 2018, 1,839 new cases of prostate cancer were diagnosed. They estimated prostate cancer to be the third most common cancer among Malaysian men, with a lifetime risk of 1 in 117.
However, the study's scope was limited to a few urology centres and a comprehensive investigation of the wider community's prevalence is lacking. Many Malaysians, especially those in rural areas, don't usually seek early medical care, which often leads to a late diagnosis of the disease. As of now, there aren't any widespread screening programmes to accurately determine how prevalent prostate cancer is within the community. As a result, Jasmine's study likely only captured those who sought care at the specific urology centres, leaving many cases undetected in the community.
The prevalence of prostate cancer is higher among Caucasians and Blacks than Asians, with a greater incidence in developed countries compared to developing ones. In Southeast Asia, it is reported at 11.2 per 100,000 men (Martin C.S. Wong, William B. Goggins Harry H.X. Wang, et al * Global Incidence and Mortality for Prostate Cancer: Analysis of Temporal Patterns and Trends in 36 Countries EUROPEAN UROLOGY 70 (2016) 862–874). Singapore, for instance, has a rising rate of 25 per 100,000 men, while Australia's rate remains steady at 120 per 100,000 men.
Challenges of traditional prostate cancer treatments and how technology is overcoming them
Traditional prostate cancer treatments, like those involving Stereotactic Body Radiation Therapy (SBRT), face several challenges. These treatments typically require an extended duration of radiation treatment, spanning over five weeks with daily sessions lasting 10 to 15 minutes, five days a week, to deliver the necessary dose to the prostate cancer site.
Additionally, these methods often result in collateral damage to nearby organs such as the bladder, urethra, and rectum. This damage can be both immediate and long-term, potentially leading to significant discomfort and a reduced quality of life for patients. Therefore, it is crucial to balance delivering an effective radiation dose with minimising harm to surrounding tissues.
Another commonly accepted traditional treatment method is brachytherapy, where radioactive seeds are implanted directly into the prostate. This method emits low-dose radiation from within the prostate, unlike external beam radiotherapy which uses external ionising radiation. Brachytherapy approach has the advantage of causing less collateral damage to the surrounding normal tissues.
Newer treatments focus on more precise targeting of the tumour to further reduce collateral damage and improve patient outcomes.

Compared to traditional Intensity-Modulated Radiation Therapy (IMRT), Stereotactic Body Radiation Therapy (SBRT) delivers the entire radiation dose in a shorter duration.
Stereotactic Body Radiation Therapy (SBRT): precision and safety in prostate cancer treatment
SBRT is an advanced technique of external beam radiation that delivers the entire radiation dose in a shorter timeframe, usually five to six days, compared to conventional Intensity-Modulated Radiation Therapy (IMRT), which requires five weeks of treatment. This method has shown success for specific grades of prostate cancer, providing high local control rates while minimising toxicity to healthy tissues.
SBRT has already proven effective in treating various types of cancer, including lung cancer and lung metastases, primary liver cancer and liver metastases, pancreatic cancer, prostate cancer, recurrent head and neck cancer, recurrent gynaecological cancers, and several other types of cancer in different parts of the body.
For low and intermediate-risk prostate cancers, SBRT has shown biochemical relapse-free survival rates of 90% to 100%, with a median follow-up of five years or more. Additionally, early evidence indicates that SBRT is as effective as brachytherapy, but with fewer side effects. SBRT works by precisely targeting prostate cancer, helped by the Urologist placing gold fiducials into the prostate to guide the treatment. Additionally, a special gel is injected into the space between the rectum and the prostate to protect the rectum from radiation damage.
What is the role of a gel-like spacer as part of the prostate cancer treatment process?
This technique involves injecting a gel to form a protective layer that separates the prostate from the front of the rectum, with the primary aim of reducing the damaging effects of radiation on the rectum. Recent abroad data has shown promising results, demonstrating a reduction in radiation proctitis rate from the usual 13.8% to just 2.9% with this method.
This notable reduction in rectal side effects allows for a higher radiation dose to the prostate, thus improving the treatment's effectiveness.
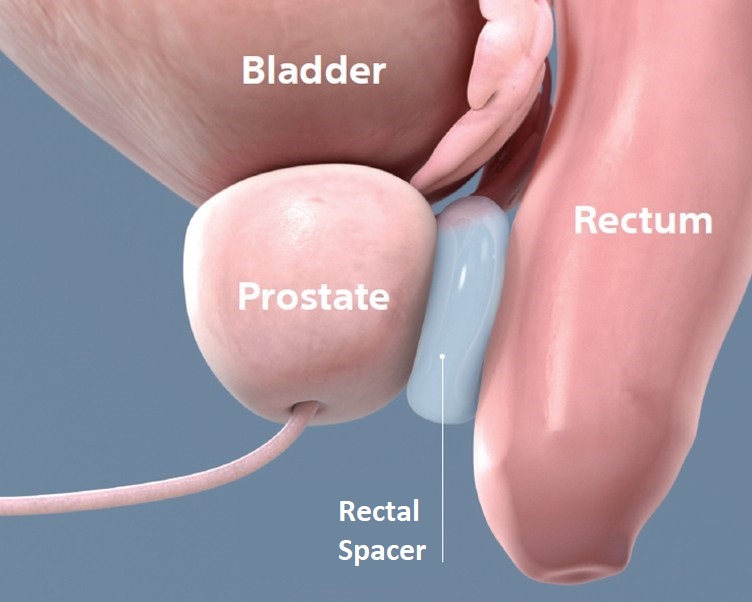
The SBRT procedure for prostate cancer involves injecting a specialised gel into the space between the rectum and prostate to reduce the damaging effects of radiation on the rectum.
How do you see the future development of health tech solutions impacting cancer treatment and patient care?
The integration of health technology into cancer treatment has played a crucial role in advancing the field and enhancing patient care. Advances in MRI imaging for prostate cancer have led to more precise and safer biopsy methods.
Advanced imaging technologies, such as Prostate-Specific Membrane Antigen (PSMA) scans, have opened new possibilities for focal therapy in prostate cancer. This approach targets specific individual prostate lesions using precise techniques like highly focused ultrasounds, lasers, electroporation, or cryotherapy. As a result, healthy surrounding tissues are preserved, minimising collateral damage. Since 2015, nearly 6,000 patient trials and 72 studies have been conducted on these newer treatment modalities.
Moreover, the range of treatments for advanced prostate cancer is increasing, with novel drugs like PARP inhibitors now available. These drugs belong to a specialised category of anti-cancer therapies that target DNA repair mechanisms.
Radioligand therapy involving agents like Lutetium 177, targets prostate cancer cells specifically, offering both diagnostic and therapeutic benefits simultaneously. This development has resulted in the creation of a new field known as “theranostics”. The primary drawback, however, is the continuous rise in healthcare costs associated with new medical solutions.
Early Detection Tips for Malaysians to Fight Cancer and Other Diseases
Early detection is the most effective way to combat prostate cancer. My advice for all men over the age of 50 is to take a simple blood test called the “Prostate Specific Antigen” test. This test is affordable and can quickly identify the 20% of men who require further investigations for early detection of prostate cancer.
The ProTect trial, one of the longest recorded trials on prostate cancer treatment conducted in the United Kingdom, demonstrated a remarkable 96 to 97 per cent survival rate for clinically localised prostate cancer over a median follow-up period of 15 years, regardless of the treatment assigned.
The encouraging news is that prostate cancer is highly treatable, and it is crucial to prioritise treatment for men with an expected lifespan exceeding 10 years. Prostate cancer at the curable stage typically manifests without any noticeable symptoms.
Therefore, it is essential not to wait until experiencing difficulties in urination or pain. Get your PSA tested and consult your general practitioner or urologist.
For elderly individuals who do not have a realistic life expectancy beyond this timeframe, a more conservative approach may be appropriate, given that only 1 out of every 7 men diagnosed with prostate cancer succumbs to the disease.
Source: CodeBlue