Expert insights by Dr Ganesalingam Kanagasabai | SJMC Consultant Gastroenterologist

What is Fatty Liver Disease (MASLD)?
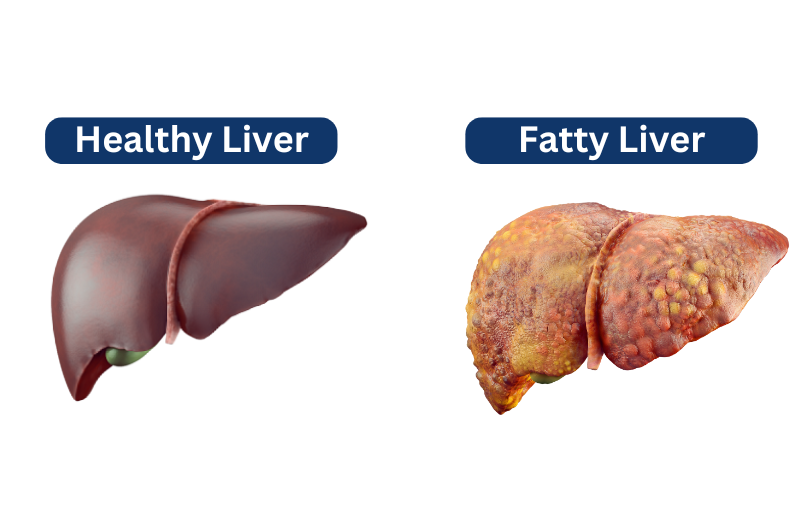
Fatty liver disease, now referred to as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), is a condition where excess fat accumulates in the liver (steatosis). This occurs when at least one cardiometabolic risk factor is present, such as obesity, diabetes, high blood pressure, or high cholesterol levels. Cardiometabolic risks are risk factors that increase the likelihood of experiencing vascular events such as a heart attack and strokes or developing diabetes.
Over time, MASLD can progress to Metabolic Dysfunction-Associated Steatohepatitis (MASH), a more severe form of liver inflammation. If left untreated, this can lead to fibrosis, cirrhosis, and liver cancer. Fatty liver disease (MASLD) is now also considered a significant risk factor for cardiovascular disease (CVD), non-liver malignancies, lung diseases, and chronic kidney disease (CKD), osteoarthritis, obstructive sleep apnea and polycystic ovary syndrome.
Risk Factors for Fatty Liver Disease (MASLD)
Fatty liver disease (MASLD) is closely linked to metabolic dysfunction, with several key factors increasing the risk of developing this condition.
1. Obesity and Unhealthy Diet
Obesity is the leading risk factor for MASLD, with Malaysia having one of the highest obesity rates in Asia. According to the National Health and Morbidity Survey (NHMS) 2023, 54.4% of Malaysian adults are overweight or obese. This is largely driven by:
✅ Diets high in ultra-processed foods, unhealthy fats, sugary drinks, and red meat
✅ Low intake of fruits and vegetables – Only 4.9% of Malaysians meet the daily recommended intake
✅ Lack of physical activity – 29.9% of Malaysians are physically inactive
Poor dietary habits and sedentary lifestyles contribute to excess fat storage in the liver, increasing the risk of MASLD.
2. Type 2 Diabetes and Insulin Resistance
Individuals with type 2 diabetes have a higher risk of fatty liver disease (MASLD) and liver damage. These individuals have excess insulin and glucose in the blood which promotes fat storage in the liver cells, leading to fat accumulation. Type 2 diabetes is also likely to:
- Accelerate liver inflammation (steatohepatitis), leading to fibrosis and cirrhosis.
- Cause oxidative stress, worsening liver damage and increase fatty liver disease (MASLD) progression.
3. High Blood Pressure and High Cholesterol
Individuals with hypertension (high blood pressure) and unfavourable cholesterol profiles have higher risk of developing liver inflammation and fibrosis.
The NHMS 2023 survey revealed that only 4.9% of Malaysians consume the recommended amount of fruits and vegetables, while 29.9% lead an inactive lifestyle—both factors contribute to high cholesterol, hypertension, and liver damage.
Regular health screenings and lifestyle modifications such as a balanced diet, exercise, and proper cholesterol management can reduce the risk of MASLD complications.
Common Symptoms of Fatty Liver Disease (MASLD)
Most people with MASLD experience no symptoms until the disease progresses to severe liver damage. By the time symptoms appear, the liver may already be in the cirrhosis or liver failure stage.
Symptoms of liver cirrhosis and liver failure include:
- yellowness of the eyes and skin (jaundice)
- bruising easily
- dark urine
- swelling of the tummy area (ascites)
- vomiting blood
- dark black tarry poo
- periods of confusion, forgetting things, mood changes or poor judgement (encephalopathy)
- itching skin
The silent nature of the disease, with little to no symptoms, often leads to late diagnosis when complications such as liver inflammation (MASH), fibrosis, cirrhosis, and liver cancer have already developed.
If you experience any of these symptoms, seek medical attention immediately.
How is MASLD detected and how can this disease be managed?
Since MASLD often shows no early symptoms, routine health check-ups are the best way to detect it early.
Tests to diagnose fatty liver disease include:
✔️ Liver Function Test (LFT) – Measures liver enzyme levels to check for liver inflammation
✔️ Abdominal Ultrasound – Detects fat accumulation in the liver
✔️ FIB-4 Score Calculation – Uses age, liver enzyme values, and platelet count to assess liver fibrosis risk
✔️ Fibroscan (Liver Stiffness Test) – A specialised ultrasound that measures liver stiffness and fat content
If a patient has a FIB-4 score above 1.3, they may be at higher risk of liver fibrosis and should consult a gastroenterologist for further evaluation.
Treatments for Fatty Liver Disease (MASLD)
The number one killer in MASLD is cardiovascular diseases, including heart attacks and strokes. It is therefore important to manage all the cardio-metabolic risk factors. Diabetes and high blood pressure must be well controlled and cholesterol medication should be prescribed if indicated. Weight reduction in overweight individuals is essential. A bodyweight reduction of ≥5% is required to reduce liver fat content, 7-10% to improve inflammation, and ≥10% to improve fibrosis. It also important to stop smoking, minimize alcohol consumption, exercise regularly and eat a healthy diet.
Patients with MASH or cirrhosis should be monitored regularly by their gastroenterologist. These patients are at an increased risk of liver cancer and should undergo regular surveillance. Patients with end stage liver failure might require a liver transplant.
The good news is that a drug known as resmetirom was approved for the treatment of MASLD in America recently, for patients with significant fibrosis in the liver. There are also several other drugs that are currently undergoing phase 3 trials. I am hopeful that resmetirom and other drugs will soon be available in Malaysia for the treatment of MASLD.
How effective are supplements in managing MASLD symptoms?
Supplements are not recommended to manage MASLD, since there is insufficient evidence of their safety profile and their effectiveness in reducing liver damage/fibrosis and liver-related outcomes in MASLD. Some supplements do have anti-inflammatory properties that might reduce liver enzymes, but this has not translated to improved liver fibrosis.
It is also important to remember that patients with MASLD are more likely to die from a heart attack, a stroke or non-liver cancer. Treatment should be focused on reducing the risk of these diseases. The one thing that might help is coffee! Coffee consumption – caffeinated or not – has been shown to have a protective association with MASLD , as it has been found to reduce liver fibrosis, death from chronic liver disease and liver cancer.
How to Prevent Fatty Liver Disease (MASLD)?
The easiest way to prevent MASLD is by adopting a healthy lifestyle. Physical activity and exercise are recommended to reduce liver fat, tailored to the individual’s preference and ability (preferably >150 min/week of moderate or 75 min/week of vigorous-intensity physical activity). Improving the quality of one’s diet (similar to the Mediterranean dietary pattern), limiting the consumption of ultra-processed food (rich in sugars and saturated fat) and avoiding sugar-sweetened beverages are highly recommended.
Specialists for Fatty Liver Disease (MASLD) | Who to Consult?
If you have fatty liver disease (MASLD) or are at risk, consult a specialist to manage your liver health effectively.
🔹 Gastroenterologist / Hepatologist – For liver function assessment, Fibroscan, and monitoring fibrosis, cirrhosis, or liver cancer.
🔹 Endocrinologist – If you have diabetes, insulin resistance, or metabolic syndrome contributing to MASLD.
🔹 Cardiologist – If you have high blood pressure, high cholesterol, or an increased risk of heart disease.
🔹 Dietitian / Nutritionist – For dietary counselling to support weight loss and improve liver health.